Before jumping into Stabilization Centre, we must know what is Severe Acute Malnutrition (SAM)?
- In children who are 6–59 months of age, severe acute malnutrition (SAM) is defined as:
- weight-for-height ≤–3 Z-score, or
- mid-upper-arm circumference <115 mm, or
- presence of bilateral oedema
Now let us move into 12 must know things about Stabilization Centre:
- Stabilization Center (SC) is a place/ward where children with Severe Acute Malnutrition (SAM) along with other issues like medical complications/poor appetite/+++ edema/IMCI danger signs are kept for stabilizing their health
- Nowadays, the name Stabilization Centre (SC) is being replaced by Inpatient Therapeutic Centre (ITC), although there are no changes in the function. But for this article we are using the term SC for our simplicity and understanding
- SC is the last place for saving life of severely acutely malnourished child
- The first place for treating children with SAM is OTC (Outpatient Therapeutic Centre). Children whose condition is worse and who cannot be treated through OTC are admitted in SC i.e. all children with SAM cannot/will not be kept in SC.
- There are certain criteria for admitting children with SAM in Stabilization Centre. Children with SAM must have at least one of the following criteria for admitting in SC. They are:
- Severe oedema (+++)
- Have medical complications
- Poor appetite (children who are only able to eat less than 1/3 of Ready to Use Therapeutic Food (RUTF) in one hour)
- One or more IMCI danger signs: unable to drink or breastfed, vomits everything, convulsions
- As the children in SC are not in good/normal stage of their health, certain actions must be taken immediately and as long as the child is in SC in order to stabilize the health of the child. These actions which are essential elements for stabilization of child’s health in SC are:
- Early initiation of feeding
- Broad spectrum antibiotic therapy
- Micronutrient supplementation
- Less use of IV fluids
- Slower rehydration
- Treatment of complications
- Health of child in SC can worsen any time, if proper care and treatment is not provided. Thus, treatment is SC is to be led by either doctor or nurses. Other paramedics may not be fully acquainted with case handling in complicated/worst case scenarios
- Different kinds of therapeutic foods are given while treating the child in SC. F-75 milk is given in the stabilization/initial phase while once health of the child is stabilized, F-100 milk is introduced
- Foods like Ready to Use Therapeutic Food (RUTF) and Ready to Use Supplementary Food (RUSF) is not given in SC.
- Admitting in SC means the child has to remain in SC unless he/she is discharged. It is similar to admitting in hospital i.e. cannot go back home unless fully cured.
- After the health of the child is stabilized, children’s should be discharged from SC or transferred to OTC (if present) for further treatment by using Therapeutic foods like RUTF.
- Children admitted in SC can only be discharged from SC (i.e. transferred to OTC) if:
- No medical complications
- Good appetite (eating more than 1/3 of RUTF in one hour)
- Lessened oedema
- No IMCI danger signs and clinically alert
- In addition, we must know that the discharge criteria for children age 6-59 months and less than 6 months are different
Children from 6-59 months should be discharged from SC if they fulfill the following criteria:
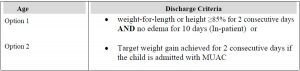
Note: Option 1 is the preferred option. Option 2 should only be referred if the health facility does not have equipment to measure height
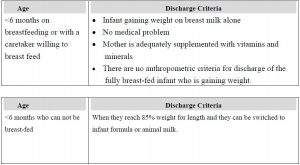
On the other hand, children age less than 6 months should be discharged if they fulfill the following criteria:
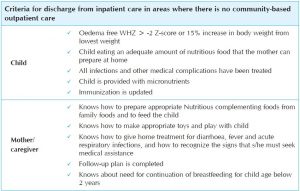
While looking holistically, we can also consider the following discharge criteria for our simplicity:
References and for further information:
WHO. Guideline: Updates on the management of severe acute malnutrition in infants and children. Geneva, World Health Organization; 2013 (http://www.who.int/nutrition/publications/guidelines/updates_management_SAM_
infantandchildren/en/)
WHO, WFP, UNSCN, UNICEF. Community-based management of severe acute malnutrition. A joint statement by the World Health Organization, World Food Programme, United Nations Standing Committee on Nutrition, United Nations Children’s Fund. Geneva, World Health Organization; 2007 (http://www.who.int/nutrition/publications/severemalnutrition/9789280641479/en/)
https://www.unicef.org/health/somalia_59738.html
https://www.ncbi.nlm.nih.gov/books/NBK190317/
http://www.who.int/elena/titles/full_recommendations/sam_management/en/index4.html
http://www.ennonline.net/fex/16/outpatient
http://www.nsp.gos.pk/stabilization
https://nrhm.gujarat.gov.in/images/pdf/nrc_guidelines.pdf
http://www.who.int/elena/titles/transition_feeding_sam/en/
http://www.open.edu/openlearncreate/mod/oucontent/view.php?id=323&printable=1
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2083726/
http://reliefpakistan.org/Stabilization%20center%20Report%20(%20KPK).pdf
Desta, K. S. (2015). Survival status and predictors of mortality among children aged 0–59 months with severe acute malnutrition admitted to stabilization center at Sekota Hospital Waghemra Zone. J Nutr Disord Ther, 5, 160.
https://motherchildnutrition.org/resources/pdf/mcn-otp-quick-ref-manual-for-hew.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746053/
https://www.fantaproject.org/sites/default/files/resources/CMAM_Training_Mod5_ENGLISH_Nov2008.pdf
http://www.ennonline.net/fex/47/nutritional