Table of Contents
What is Postpartum Hemorrhage (PPH)?
- The World Health Organization (WHO) defines postpartum hemorrhage (PPH) as ‘blood loss that exceeds 500 milliliter (ml) after a vaginal birth or 1000 ml after a cesarean section.’
- Postpartum hemorrhage, or PPH, occurs when a woman has significant bleeding soon after delivering baby.
- Postpartum hemorrhage is a severe yet uncommon condition after the birth of a child.
- PPH often manifests within 24 hours of delivery, however it can sometimes appear up to 12 weeks after delivery.
- Moreover, it is defined as any quantity of vaginal bleeding after delivery that result in abnormal vital signs or a 10% decrease in hemoglobin from the baseline.
- Atony of the uterus, retained tissue, genital tract tears, coagulation issues, and uterine rupture are the main causes of PPH.
Key Facts
- PPH, which accounts for more than 25% of yearly fatalities, is the main cause of maternal mortality and morbidity worldwide.
- Globally, PPH affects roughly 14 million women annually and causes 70,000 maternal deaths.
- According to WHO figures, PPH causes more than 100,000 maternal fatalities annually globally, 60% of which occur in poor nations.
- Even if a woman survives, she may have permanent reproductive disabilities and frequently requires emergency surgical procedures to stop the bleeding.
- The majority (99%) of maternal deaths caused by postpartum vaginal hemorrhage occur in low- and middle-income countries.
Causes of Postpartum Hemorrhage
The four T’s mnemonic can be used to identify and address the four most common causes of PPH (uterine atony [Tone]; retained tissue or invasive placenta [Tissue]; laceration, hematoma, inversion, rupture [Trauma];and coagulopathy [Thrombin]).
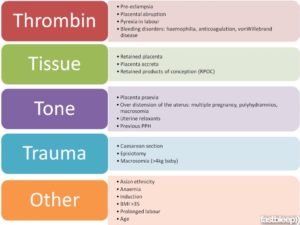
1. Uterine atony
- Uterine atony, also known as uterine tone, occurs when the uterus is soft and weak after childbirth, leading to insufficient contractions of the uterine muscles to close the blood vessels connected to the placenta.
- As a result, there is a continuous loss of blood after delivery.
2. Retained placental tissue
- Retained placental tissue refers to a condition where the entire placenta does not separate from the uterine wall.
- This may be due to underlying placental conditions that affect the uterus’s ability to contract after delivery.
3. Uterine trauma
- Bleeding may occur due to uterine trauma, which is the result of damage to the vagina, cervix, uterus, or perineum during delivery.
- The use of instruments such as forceps or vacuum extraction during childbirth can increase the risk of uterine trauma.
- In some cases, bleeding may occur hours or days after delivery due to the formation of a hematoma in a concealed area.
4. Blood clotting condition
- If a person has a blood clotting condition like thrombin or a pregnancy-related condition such as eclampsia, it can interfere with the body’s ability to clot, leading to uncontrolled bleeding even from a small wound.
Types of Postpartum Hemorrhage
Primary PPH:
- This happens within the time frame of 24 hours to 12 weeks following childbirth.
Secondary PPH:
- This occurs between 24 hours and 12 weeks after childbirth.
- It is less common than primary PPH and usually occurs due to infections, retained placental tissue, or other complications related to childbirth.
Symptoms
The symptoms of postpartum hemorrhage (PPH) may vary in severity and can include:
- Heavy or prolonged bleeding from the vagina, with or without clots.
- Increased heart rate or heart palpitations.
- A drop in blood pressure or experiencing lightheadedness or dizziness
- Pale skin or a pale complexion.
- Feeling lightheaded or dizzy.
- Shortness of breath or difficulty breathing.
- Abdominal pain or discomfort.
- Discomfort or inflammation in the perineal region
- Decreased urine output.
- Fatigue or weakness.
- It is important to note that some bleeding is normal after childbirth, but if bleeding becomes heavy or prolonged, or if any of the above symptoms are present, medical attention should be sought immediately.
Stages of Postpartum Hemorrhage
Postpartum hemorrhage (PPH) is typically classified into four stages based on the amount of blood loss and the severity of symptoms:
Stage 1
- Mild PPH involves blood loss of 500-1000 ml (less than 20% of blood volume)
- Mild symptoms such as increased heart rate, mild abdominal pain or discomfort, and slight decrease in blood pressure.
Stage 2
- Moderate PPH involves blood loss of 1000-2000 ml (20-40% of blood volume)
- More prominent symptoms such as increased heart rate, decreased blood pressure, and more severe abdominal pain.
Stage 3
- Severe PPH involves blood loss of more than 2000 ml (more than 40% of blood volume)
- Severe symptoms such as rapid heart rate, low blood pressure, confusion, shortness of breath, and signs of shock.
Stage 4
- Refractory PPH involves continued bleeding despite attempts to control it and may require emergency interventions such as surgery or blood transfusion.
High Risk Groups for Postpartum Hemorrhage
- There are varying degrees of risk for postpartum hemorrhage among women, and some factors that may increase this risk include certain medical conditions.
- Placental abruption, which refers to the detachment of the placenta from the uterus, as well as placenta previa, which occurs when the placenta covers or is near the cervix opening, are two such conditions.
- Over distended uterus, which can result from too much amniotic fluid or a large baby, multiple-baby pregnancy, high blood pressure disorders during pregnancy, many previous births, prolonged labor, infection, obesity, and use of forceps or vacuum-assisted delivery can all contribute to an increased risk.
- Women of Asian or Hispanic ethnicity may also be at a higher risk for postpartum hemorrhage.
Risks and Seriousness of Postpartum Hemorrhage
- Shock: Severe blood loss can lead to shock, which can cause organ failure, low blood pressure, and even death.
- Anemia: Excessive blood loss can cause anemia, which can lead to fatigue, weakness, and other complications.
- Infection: PPH can increase the risk of infection, particularly if the cause of bleeding is due to retained placenta or other tissue.
- Need for blood transfusion: Severe blood loss may require a blood transfusion, which carries its own risks such as allergic reactions or infections.
- Long-term health consequences: In some cases, PPH can lead to long-term health consequences such as infertility, pelvic pain, or scarring.
- Psychological impact: PPH can also have a psychological impact on the mother, such as fear of future pregnancies or post-traumatic stress disorder.
Diagnosis
- Assessment of the amount and pattern of vaginal bleeding, including the measurement of blood loss.
- Monitoring vital signs such as heart rate, blood pressure, and oxygen saturation.
- Blood tests to assess the patient’s blood count and clotting function.
- Ultrasound or other imaging studies to assess the uterus and other organs for signs of bleeding or trauma.
Prevention
- Active management of the third stage of labor, which involves administering medication to help the uterus contract and deliver the placenta.
- Close monitoring of patients with risk factors for PPH, such as those with previous PPH or multiple pregnancies.
- Prompt identification and treatment of conditions that increase the risk of PPH, such as placental abnormalities or high blood pressure disorders.
- Consideration of prophylactic measures such as administration of medications or blood transfusions in high-risk patients.
Treatment
- Administration of medications to help the uterus contract and reduce bleeding, such as oxytocin, misoprostol, or carboprost.
- Manually remove the placenta or any remaining products of conception from the uterus to treat postpartum hemorrhage.
- Surgical intervention, such as uterine artery embolization or hysterectomy in severe cases.
- Blood transfusions may be administered to replenish the blood volume that has been lost
- Supportive measures such as oxygen therapy and intravenous fluids to stabilize vital signs.
References and For More Information
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8640320/
https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-019-4646-9
https://www.frontiersin.org/articles/10.3389/fgwh.2022.1020163/full
https://my.clevelandclinic.org/health/diseases/22228-postpartum-hemorrhage
https://www.stanfordchildrens.org/en/topic/default?id=postpartum-hemorrhage-90-P02486
https://emedicine.medscape.com/article/275038-overview
https://www.uptodate.com/contents/overview-of-postpartum-hemorrhage
https://www.ncbi.nlm.nih.gov/books/NBK499988/
https://ihub.scot/media/5690/pph-4-stage-practical-guide_final.pdf