Table of Contents
What is Antimicrobial Resistance (AMR)?
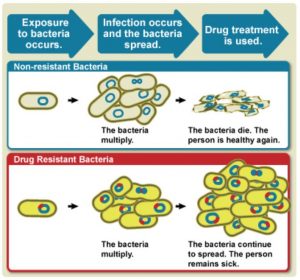
- Antimicrobial Resistance (AMR) is the ability of microorganisms (bacteria, virus, fungi, parasites etc.) to grow and multiply despite their exposure to antimicrobial substances which are designed to inhibit their growth.
- Antimicrobial resistance is the effect of microorganisms/microbe to resist the effect of antimicrobial drug.
- Antimicrobials including- antibiotics, antivirals, antifungals and antiparasites – are medicines used to prevent and treat infections/infectious disease in humans, animals and plants.
- Antimicrobial resistance refers to the natural ability of microorganisms to evolve genetically to counter/resist the drugs.
- It is a condition where a microbe/pathogen has resistance gene so that the antimicrobial drug cannot kill it.
- Antimicrobial resistance makes infections harder to treat and increasing the risk of disease spread, severe illness and death.
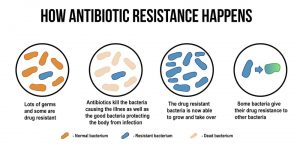
- Antimicrobial resistance takes place, once microorganisms such as bacteria, viruses, fungi, and parasites transform (make changes inside their genomes) when they are exposed to antimicrobial drugs (antibiotics, antifungals, antivirals, antimalarials, and antihelminthics). This transformation ultimately results in ineffectiveness of the antimicrobial drugs.
- Note: Only those microorganisms which can make changes inside their genomes, when exposed to the antimicrobial drug, can survive the effect of drug. As a result, these microorganisms become resistant to the (specific) antimicrobial drug.
- Antimicrobial resistance is the wider term for a resistance in diverse types of microorganisms which ultimately comprises the effect of antibacterial, antiviral, antiparasitic and antifungal drugs. Antimicrobial resistance also comprises of antibiotic resistance.
- Microorganism that are resistant to the antimicrobial drugs are called ‘super bugs.’ These microorganism/superbugs are heavily resilient against antimicrobial drugs.
- Antimicrobial resistance is a most threatening situation because medicines will be ineffective against resistant organisms. As a result, the infections will persist, spread to others, and forces huge expenditures to individuals and society in terms of health and the environment.
- Therefore, antimicrobial resistance is an immediate, serious, complex and expensive public health problem. It is a growing global threat to the entire living beings.
Present situation of Antimicrobial Resistance (AMR):
- Accelerating antimicrobial resistance is a life-threatening problem globally, with several health administrations building the issue an urgency for upcoming progress and research.
- According to the Centers for Disease Control and Prevention , each year in the United States at least 2.8 million antibiotic-resistant infections occur, and more than 35,000 people die as a result of antibiotic resistant bacteria(CDC, 2019).
- In 2016, 490, 000 people developed multi-drug resistant TB globally, and drug resistance is starting to complicate the fight against HIV and malaria, as well. (WHO 2020).
- According to European Centre for Disease Prevention and Control, every day 1 in 3 patients receive at least one antimicrobial drug. Some of these are usually unnecessary and lead to the spread of antimicrobial resistance mechanism.
- WHO’s new Global Antimicrobial Surveillance System (GLASS) discloses an extensive incident of antibiotic resistance among 500,000 people with assumed bacterial infections through 22 countries.
- There is a desperate necessity for new operational antimicrobials and new antibiotics to be developed.
- Moreover, it is necessary to understand the mechanisms and epidemiology of the resistant pathogens currently existing in the community in order to develop new antibiotics/antimicrobials.
- According to World Health Organization (WHO), without urgent action, we are heading towards a “post-antibiotic era in which common infections and minor injuries (which have been treatable for decades) can once again kill”.
- Most frequently informed resistant bacteria or bacterium were Escherichia coli , Klebsiella pneumoniae , Staphylococcus aureus , and Streptococcus pneumoniae, tracked by Salmonella. The system does not take in data on resistance of Mycobacterium tuberculosis , that causes tuberculosis (TB), as WHO has been tracing it ever since 1994 and providing yearly updates in the Global tuberculosis report .
- In the US, the CDC estimated the cost of AMR as $55 billion per year overall: $20 billion in excess for direct healthcare costs, with additional society costs for lost productivity as high as $35 billion a year (CDC, 2013)
What is the Difference between Antimicrobial Resistance and Antibiotic Resistance?
Antimicrobial Resistance |
Antibiotic resistance |
| Antimicrobial resistance is the resistance of microorganisms (bacteria, virus, fungi, parasites etc.) to different antimicrobial drugs and all antimicrobial agents. | Antibiotic resistance is the resistance of bacteria to the antibiotics. |
| Antimicrobial resistance is a broader term, encompassing resistance to drugs to treat infections caused by other microbes as well, such as parasites (e.g. malaria), viruses (e.g. HIV) and fungi (e.g. Candida). | Antibiotic resistance is a narrow term referring to the resistance to antibiotics in bacteria-based diseases such as tuberculosis etc. |
| Antimicrobial resistance occurs when different microorganism (bacteria, virus, fungi, parasite etc.) change in response to the antimicrobial agents. | Antibiotic resistance occurs when bacteria change in response to the use of antibiotic medicines. |
Antimicrobial Resistance Mechanism?
- AMR takes place when the DNA of micro-organisms mutates and when resistant traits are exchanged between them.
- The drug expert David Cox explains what happens at the molecular level:
- Such mutations can prevent an antibiotic entering the bacteria cell at all, altering the target molecules so that they don’t bind to the antibiotic anymore, or enhancing the efficiency of efflux mechanisms within the bacteria which allow it to simply pump a drug back out again. Certain genes, if acquired, can actively degrade antibiotics, limiting their effectiveness once they’ve entered the cell. (Source: https://www.richarddawkins.net/2016/04/antimicrobial-resistance-what-you-need-to-know/)
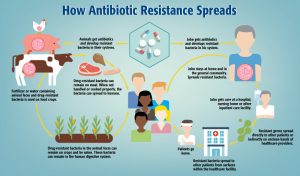
How does Antimicrobial Resistance Spread?
What are the Causes of Antimicrobial Resistance?
- Natural (biological) phenomenon
- Inappropriate/irrational use of antimicrobials
- Inadequate diagnostics and hospital factors
- Unnecessary use of antimicrobial drugs in agriculture
- Poor hygiene and sanitation
Brief description of these reasons/causes for accelerated increase of Antimicrobial resistance are:
1. Natural (biological) phenomenon:
- The development of resistant strain is an inevitable consequence of natural selection. Antimicrobial resistance is a natural phenomenon that occurs when microorganisms are exposed to antibiotic drugs.
- Microscopic organism adapts to their surroundings and transform in various ways that make certain of their survival. If some disruptions occur in their ability to grow, such as exposure to an antimicrobial drug, genetic alteration can occur. This genetic alteration will increase the microorganism resistance/bacterial resistance and will help the organism (resistant strain) to survive.
- Microorganism resistance/bacterial resistance happens in several ways and results in increment of AMR.
a) Selective Pressure
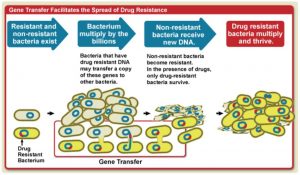
b) Mutation
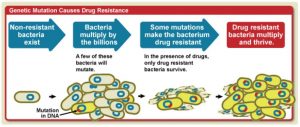
c) Gene transfer
Apart from the natural resistance mechanism of microorganisms to antimicrobial drugs, there are different factors that accelerate the increase of AMR.
In most of the cases, health sector is mainly held responsible for AMR. However, if we view and treat antimicrobial resistance solely as a health sector problem, we will be neglecting behavioural, environmental, agricultural, economic and social contributions to AMR. Moreover, overuse of antimicrobials in both animals and humans contributes to antimicrobial resistance.
2. Inappropriate/irrational use of antimicrobials
- Increasing use of Over-the-Counter (OTC) drugs/self-medication.
- Misuse and overuse of antimicrobials.
- Antibiotic overuse.
- Substantial consumption of antimicrobials in ill patients can deteriorate the problem causing AMR. The wide use of antimicrobials and close interaction between ill patients generate a productive environment for the spread of antimicrobial-resistant germs.
- Examples of misuse: Antibiotic use during non-bacterial infection/viral infection like cold and flu.
3. Inadequate diagnostics and hospital factors:
- Inappropriate antimicrobial/antibiotic prescription: Healthcare suppliers or providers use inadequate or lacking information to detect an infection and consequently recommend an antimicrobial just in case or prescribe a broad-spectrum antimicrobial while a particular antibiotic might be healthier.
- Widespread and prolonged use of antimicrobials for therapy and prophylaxis.
- Prescribing antibiotics during viral infection.
- Poor infection control in health facilities.
- Lack of rapid laboratory tests which may lead to wrong use of drugs.
4. Unnecessary use of antimicrobial drugs in agriculture:
- Antibiotics are haphazardly used in farm animals as “growth promoters” or mass prophylaxis to prevent illness rather than just to treat sick animals.
- Researchers also consider that the practice of adding antibiotics to agricultural food encourages drug resistance.
- Farmers also use antibiotics in crops to prevent fire blight.
5. Poor hygiene and sanitation:
- Poor infection control, inadequate sanitary conditions, and inappropriate food-handling also increase the spread of antimicrobial resistance.
- Inadequately treated waste streams from households, hospitals and farms using antimicrobials release antimicrobials into the environment. Release of antimicrobials in the environment encourage the growth of resistant organisms. These waste streams can also release resistance genes and resistant microorganisms into the environment, where they can act as reservoirs for genetic exchange and further development of resistance.
- Release of large amount of antibiotics in wastewater.
6. Other causes:
- Lack of compliance in use of antibiotics by the patient i.e. not completing the full dose as prescribed.
Consequences/Effects of Antimicrobial Resistance?
- Antimicrobial resistance threatens the effective prevention and treatment of an increasing range of infections caused by bacteria, parasites, viruses, and fungi.
- AMR decreases our ability to treat or fight with common infectious disease which will later result in prolonged illness, disability and death.
- The Review on Antimicrobial Resistance (AMR) determined that, left unchecked, in the next 35 years antimicrobial resistance could kill 300,000,000 people worldwide and stunt global economic output by $100 trillion.
- In fact, if the current trend is not altered, antimicrobial resistance could become the world’s single greatest killer, surpassing heart disease or cancer.
- Anti-microbial resistance causes resistance to harmful microbes i.e. microbial infections are not effectively treated in the long run.
- AMR heavily effects not only on human beings but also equally on animals’ health which seriously affects a nations food security.
- The uprising of anti-microbial resistance increases the cost more financial resources on treatment and research activities. It also increases length of hospital stay of the infected people, need of specialized equipment, additional tests and expensive antimicrobial drugs.
- Increasing Antimicrobial resistance leaves us with limited choice of antimicrobial drugs.
- Lack of effective antimicrobial use for prevention and treatment of serious infections creates very high risk for medical procedures such as organ transplantation, cancer chemotherapy, diabetes management and major surgery (for example, cesarean sections or hip replacements).
- AMR creates a demand of complex and expensive antimicrobial drugs, even for simple microbial (bacteria, virus, fungi and parasites) infections.
- Antimicrobial resistance (AMR) increases cost and expenditure of the people due to lengthier hospital stay, additional tests and use of expensive antimicrobial drugs.
- Accelerating resistance cause the rise of various modern AMR bacteria and it might be a global public health issue.
- Resistance increasingly affects neonatal health, as common infections cure might be extremely difficult.
- Negative impact on the global economy due to elevated health costs.
- Hinders productivity due to absence in a working pattern.
- AMR negatively affects food safety, food security and economic well-being of people.
Antimicrobial Resistance and COVID-19

What are the Preventive and Mitigation Measures for Antimicrobial Resistance?
- Decrease excess and irrational use of antibiotics and other antimicrobial drugs.
- Prevent severe infections so that you are less exposed to antimicrobial drugs.
- The Collaborative and coordinated approach across countries to identify, inhibit, minimize the spread and react to AMR threats from the community to national levels.
- All countries need to take antimicrobial stewardship and make national action plans on AMR.
- Strengthening Antimicrobial stewardship/Antibiotic stewardship program i.e. programs to measure and improve how antibiotics are prescribed by clinicians and used by patients).
- Greater innovation and investment are required in research and development of new antimicrobial medicines, vaccines, and diagnostic tools.
- More research should be done to know the present situation and the ways to overcome AMR.
- Appropriate prescribing of drugs by the health care personnel.
- Community education and awareness regarding AMR at the local and national level.
- The health providers should appropriately prescribe antibiotics so that an individual does not develop antibiotic resistant bacteria.
- Strong surveillance system by every health organizations to report on exact population affected by resistance and ways to combat.
- Action to combat antimicrobial resistance also requires prescribers, users and regulators of antimicrobials in human, animal and environmental health work together.
Likewise, CDC collaborates to support global action on AMR. CDC shares expertise and deploys experts to investigate and contain resistance outbreaks, and assists other countries as they:
- Implement infection prevention and control programs, and antibiotic stewardship programs in healthcare settings
- Establish or strengthen national tracking systems to respond rapidly to outbreaks, identify emerging pathogen, and track trends.
- Enhance laboratory capacity to detect and report resistance.
- Develop and implement national action plans to address the threat of antimicrobial resistance.
WHO response on Antimicrobial Resistance:
A global action plan on antimicrobial resistance, including antibiotic resistance, was endorsed at the World Health Assembly in May 2015. The global action plan aims to ensure prevention and treatment of infectious disease with safe and effective medicines.
The “Global action plan on antimicrobial resistance” has 5 strategic objectives:
- To improve awareness and understanding of antimicrobial resistance.
- To strengthen surveillance and research.
- To reduce the incidence of infection.
- To optimize the use of antimicrobial medicines.
- To ensure sustainable investment in countering antimicrobial resistance.
Conclusion:
Antimicrobial resistance is an increasingly serious threat to global public health that requires action across all government sectors and society. It threatens the effective prevention and treatment of an ever-increasing range of microbial infections. Increasing antimicrobial resistance will seriously compromise the success of major surgeries and cancer chemotherapies.
Antimicrobial use is essential to food security, to our well-being, and to animal welfare. However, the misuse of these drugs, associated with the emergence and spread of antimicrobial resistant microorganism, places everyone at great risk.
Therefore, it is necessary to strengthen and harmonize the AMR surveillance through the development of agreed epidemiological and microbiological methods and better coordination between different stakeholders.
References and For More Information:
https://www.who.int/features/qa/75/en/
https://www.biomedcentral.com/collections/antimicrobialresistance
https://www.niaid.nih.gov/research/antimicrobial-resistance-causes
https://www.who.int/mediacentre/news/releases/2018/antibiotic-resistance-found/en/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4768623/
https://www.up.ac.za/news/post_2059317-antimicrobial-resistance-a-global-concern-
https://www.cdc.gov/features/antibiotic-resistance-global/index.html
https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance
https://www.ecdc.europa.eu/en/antimicrobial-resistance
https://www.paho.org/en/topics/antimicrobial-resistance
https://www.who.int/en/news-room/fact-sheets/detail/antimicrobial-resistance
https://www.paho.org/en/documents/infographic-antimicrobial-resistance-and-covid-19
https://www.nature.com/subjects/antimicrobial-resistance
https://www.idsociety.org/public-health/antimicrobial-resistance/antimicrobial-resistance/
https://www.niaid.nih.gov/research/antimicrobial-resistance
https://www.cdc.gov/drugresistance/index.html
https://www.who.int/health-topics/antimicrobial-resistance
https://www.richarddawkins.net/2016/04/antimicrobial-resistance-what-you-need-to-know/
https://www.cdc.gov/drugresistance/about.html
https://www.cdc.gov/antibiotic-use/community/about/antibiotic-resistance-faqs.html
https://www.health.harvard.edu/blog/drug-resistant-bacteria-a-growing-health-problem-201309176677
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4768623/