Table of Contents
What is Epilepsy?
- Epilepsy is a neurological (Central Nervous System) disorder where the brain activity becomes abnormal, leading to seizures or periods of unusual sensation, behavior and sometimes loss of awareness.
- Epilepsy is a disorder of the brain characterized by repeated seizures.
- It is a common condition that affects brain and causes frequent seizures- burst of electrical activity in the brain.
- Epilepsy is a long-term, non-communicable condition of the central nervous system.
- Here the abnormal brain activity results in seizures or episodes of unusual behavior, feelings, and occasionally loss of consciousness.
- Recurrent seizures are the defining feature of epilepsy.
- Seizures are brief bursts of spontaneous movement that might affect either a portion of the body (partial) or the entire body (generalized)
- Seizure can occasionally be followed by loss of consciousness and control over bowel or bladder function.
Key Facts
- Epilepsy affects about 50 million individuals worldwide, making it one of the most prevalent neurological conditions worldwide.
- People with epilepsy make up over 80% of the population in low- and middle-income nations.
- It is estimated, up to 70% of epilepsy sufferers could avoid seizures if their condition was correctly identified and treated.
- Epilepsy sufferers have an up to three times greater chance of premature death than the general population
- In low-income nations, 75% of epilepsy sufferers do not receive the necessary treatment and care.
- People with epilepsy and their families encounter stigma and discrimination in many parts of the world.
Causes of Epilepsy
- Epilepsy is not contagious.
- Despite the fact that various underlying diseases can cause it, the origin of the disease is still unclear in 50% of the cases.
- The causes of epilepsy can be categorized as: structural, genetic, infectious, metabolic, immunological, and unknown.
- Some of the common causes of Epilepsy are:
- Brain injury brought on by perinatal or antenatal conditions, such as low birth weight, trauma at birth, or oxygen deprivation;
- Birth defects or genetic disorders with corresponding brain deformities;
- Severe head injury;
- Brain infections including meningitis, encephalitis, or neurocysticercosis;
- Strokes that reduce the amount of oxygen reaching the brain;
- Drug abuse;
- Some hereditary abnormalities;
- Tumors in the brain.
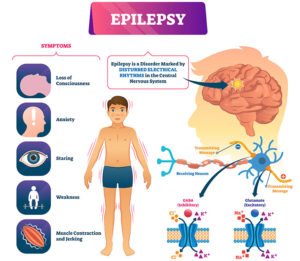
Signs and Symptoms of Epilepsy
- Temporary confusion/perplexity
- A bout of staring
- Rigid muscles
- Jerky, uncontrollable arm and leg movements, known as ‘fit’
- Loss of awareness or consciousness
- Psychological signs like worry, terror, or déjà vu
- Becoming stiff
- Collapsing
Risk Factors of Epilepsy
Age
- Although epilepsy can develop at any age, it is most frequently seen in children and older individuals.
Family history
- If there is a family history of epilepsy, there is high chance in the off springs as well.
Head trauma
- Some cases of epilepsy are caused by head injuries due to accidents and injuries
Stroke and many vascular conditions
- Damage to the brain from a stroke or other vascular (blood vessel) condition may result in epilepsy.
- In elderly persons, dementia can raise the risk of epilepsy.
Brain infections
- Risk can be raised by illnesses like meningitis, which can result in inflammation of the brain or spinal cord.
Having seizures during childhood
- Seizures and high fevers in children are sometime associated and may develop the risk of epilepsy
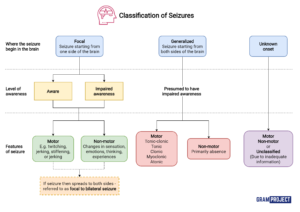
Types of Seizure During Epilepsy
Seizures are basically classified into focal or generalized seizures, depending upon how and where the abnormal brain activity begins.
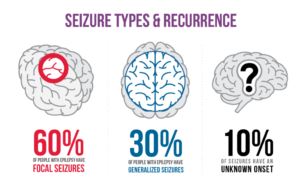
1. Focal seizures
Seizures resulting from abnormal activity in just one area of the brain
a. Focal seizures without loss of consciousness
-
- Known as simple partial seizure
- Does not result in loss of consciousness.
- It may alter emotion or change the way things look, smell, feel, taste or sound.
b. Focal seizures with impaired awareness
-
- Known as complex partial seizure
- Results in loss of consciousness or awareness
2. Generalized seizures
Seizures that affect all areas of the brain. Six types:
a. Absence seizures
- Occurs mainly in children.
- Characterized by staring into space with or without subtle body movements such as eye blinking or lip smacking and only last between 5-10 seconds.
b. Tonic seizures: Causes stiff muscles and may affect consciousness.
c. Atonic seizures: Causes loss of muscle control. Also known as ‘Drop seizures’
d. Clonic seizures: Causes repeated or rhythmic jerking muscle movements.
e. Myoclonic seizures: Occurs as sudden brief jerks or twitches
f. Tonic-clonic seizures: Causes abrupt loss of consciousness and body stiffening, twitching and shaking.
When to Consult a Doctor
Anywhere outside of hospital setting, we must call the ambulance/doctor if someone:
- Is having seizure for the first time
- Has seizures for more than 5 minutes
- Has lot of seizures in a row
- Breathing/consciousness does not return even after the seizure stops
- A person is injured during seizure
- Has breathing problems
Diagnosis
- A physician determines whether a patient has epilepsy based on their symptoms, physical examination findings, and the outcomes of tests such an electroencephalogram (EEG), computed tomography (CT or CAT scan), or magnetic resonance imaging (MRI).
- It’s crucial to correctly diagnose both the type of epilepsy and the type of seizures. Seizures fall into a number of broad categories, and the majority of them are linked to certain varieties of the condition.
Prevention of Epilepsy
- About 25 percent of epilepsy cases can be prevented.
- The best strategy to stop post-traumatic epilepsy is to prevent head injuries.
- Proper prenatal care can lower the number of new cases of epilepsy brought on by birth trauma.
- The risk of febrile seizures can be decreased by using medications and other techniques to lower a feverish child’s body temperature.
- The reduction of cardiovascular risk factors, such as actions to prevent or control high blood pressure, diabetes, and obesity, as well as abstaining from tobacco and excessive alcohol use, is the main goal of the prevention of epilepsy associated with stroke.
- The prevalence of epilepsy, such as those brought on by neurocysticercosis, can be decreased globally by the elimination of parasites in these environments and education about how to prevent infections.
Treatment
- The primary treatment involves – anti-epileptic medications
- Brain surgery to remove a tiny portion of the epileptic brain.
- An procedure to implant a tiny electrical device inside the body to regulate/control seizures
- A special diet plan (the ketogenic diet) that helps reduce seizures
WHO Response
- Epilepsy is acknowledged by WHO and its partners as a significant public health issue.
- The Global Campaign Against Epilepsy was organized by WHO, the International League Against Epilepsy (ILAE), and the International Bureau for Epilepsy (IBE) in order to “bring the disease out of the shadows,” to improve knowledge about it, increase public and private efforts to provide better care, and lessen the disease’s effects.
- The World Health Assembly (WHA) resolution on the global burden of epilepsy (WHA68.20) was accepted in 2015.
- The Resolution calls on Member States to fight epilepsy and its effects in a concerted manner.
- Numerous initiatives have been undertaken to close the treatment gap and lower the morbidity of epilepsy sufferers, train and educate medical personnel, combat stigma, find potential prevention methods, and create models integrating epilepsy care into regional health systems.
- These projects have demonstrated that there are straightforward, affordable methods to treat epilepsy in low-resource situations by combining numerous novel approaches.
- These initiatives aimed to improve the capacity of community-based primary care and nonspecialist healthcare practitioners to identify, manage, and follow up on epilepsy patients.
References and For More Information
https://www.who.int/news-room/fact-sheets/detail/epilepsy
https://www.nhs.uk/conditions/epilepsy/
https://www.healthline.com/health/epilepsy
https://www.ninds.nih.gov/health-information/disorders/epilepsy
https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Epilepsy
https://www.epilepsy.com/what-is-epilepsy
https://www.webmd.com/epilepsy/guide/epilepsy-causes
https://www.mayoclinic.org/diseases-conditions/epilepsy/symptoms-causes/syc-20350093
https://www.cdc.gov/epilepsy/about/types-of-seizures.htm