Table of Contents
Introduction:
- The Health Belief Model (HBM) is a psychological model that attempts to explain and predict health behaviors.
- It is a methodical tool that researchers or experts often use to determine or forecast human behaviors towards health.
- This is done by focusing on the attitudes and beliefs of individuals.
- Familiarizes theories from behavior disciplines to inspect health complications.
- HBM is based on following assumptions or predictions:
- An individual desire or wants to evade illness, or inversely get well in case of current illness.
- An individual believes that an exact health act might avoid, or treat illness. Eventually, a person’s opinions or views on the merits and demerits related to health manners will determine the health action taken to cure or prevent illness.
Historical Origin of HBM:
- Health Belief Model is by far the most commonly used theory in health education and health promotion.
- During the development of HBM, social psychologists were asked to explain why people do not participate in health behaviors (Rosenstock, 1960; 1966)
- The model was developed in 1950’s as a way to explain why medical screening programs offered by US Public Health Service were not successful. Later it was restructured in 1980s.
Components of Health Belief Model (HBM):
- There are six components of HBM.
- The first four components are established as the original beliefs of the HBM while the last two are more regarded as the research about the HBM developed. The six components are:
-
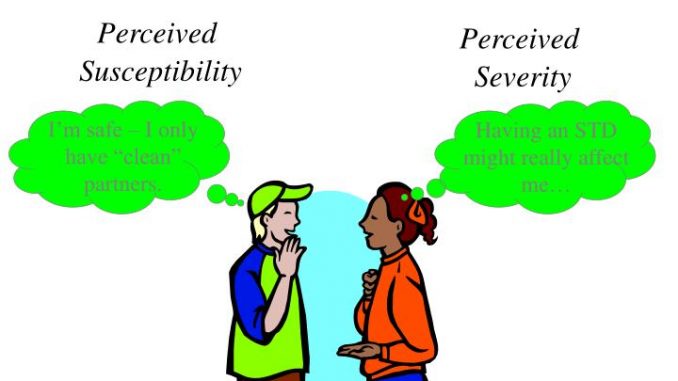
- Perceived Susceptibility
- Perceived Severity
- Perceived benefits
- Perceived barriers
- Cues to Action
- Self-efficacy

1. Perceived susceptibility:
- This refers to a person’s personal view of the risk of gaining an illness or disease. It is an individual’s perception of her or his risk of contracting a health condition
- There is extensive dissimilarity in a person’s emotional state of own susceptibility to an illness or disease.
- The person ask himself/herself the question: How likely an individual think that he/she are about to have a current health issue?
2. Perceived severity:
- It refers to an individual’s perception of the seriousness of a health condition if left untreated.
- This reflects to a person’s feelings on the urgency of contracting an illness or disease (or leaving the illness or disease untreated).
- There is varied dissimilarity in a person’s emotional state of brutality, and frequently a person reflects the health consequences (e.g., death, disability) and social consequences (e.g., family life, social relationships) when estimating the severity.
- The person ask himself/herself the question: How serious is a health problem in the current situation?
- Triggering factors for perceived severity are alarming symptoms, advice from family or friends, messages from the media, disruption of work or play.
3. Perceived benefits:
- It refers to the perceived effectiveness of taking action to improve a health condition
- The path of action plan a person takes in inhibiting (or curing) illness or disease be dependent on reflection and evaluation of mutually perceived susceptibility and perceived benefit, such that an individual would agree on the acclaimed health action if it was observed as beneficial.
- The person ask himself/herself the question: In what manner does the suggested behavior lessen the possibilities related to a present health problem?
4. Perceived barriers:
- It refers to the perceived impediments to taking action to improve a health condition.
- This denotes to a person’s frame of mind on the complications of carrying out a suggested health action.
- Extensive variation exists in a person’s mental state of obstructions, or disorders, which leads to a cost/benefit analysis.
- The person evaluates the effectiveness of the actions in contradiction of the perceptions that it may possibly be costly, hazardous (e.g., side effects), unpleasant (e.g., painful), time-consuming, or untimely.
- The person ask himself/herself the question: What are the possible adverse aspects of performing currently recommended behavior?
5. Cues to action:
- Cues to action refers to the inducement necessary to generate the decision-making process to admit a recommended health action.
- These reminders can be internal (e.g., chest pains, wheezing, etc.) or external (e.g., advice from others, illness of family member, newspaper article, etc.).
- Internal and external events can activate actions and change in behavior
- These are the factors, which cause an individual to change, or want to change? (Not scientifically considered)
6. Self-efficacy:
- Self-efficacy refers to the self- confidence in one’s ability to take action.
- This brings up to the level of a person’s confidence in his or her ability to productively implement a behavior.
- It is one’s conviction that he/she can successfully execute the behavior required to produce the outcomes.
- This conception was added to the model in recent times in mid-1980.
- Self-efficacy is a paradigm in several behavior theories. For instance, it openly relates to whether a person carries out the preferred behavior.

Application of Health Belief Model (HBM):
1. Perceived Susceptibility: Youth believe they can get STIs or HIV or create a pregnancy.
2. Perceived Severity: Youth believe that the consequences of getting STIs or HIV or creating a pregnancy are significant enough to try to avoid.
3. Perceived Benefits: Youth believe that the recommended action of using condoms would protect them from getting STIs or HIV or creating a pregnancy.
4. Perceived Barriers: Youth identify their personal barriers to using condoms (i.e., condoms limit the feeling or they are too embarrassed to talk to their partner about it) and explore ways to eliminate or reduce these barriers (i.e., teach them to put lubricant inside the condom to increase sensation for the male and have them practice condom communication skills to decrease their embarrassment level).
5. Cues to Action: Youth receive reminder cues for action in the form of incentives (such as pencils with the printed message “no glove, no love”) or reminder messages (such as messages in the school newsletter).
6. Self-Efficacy: Youth confident in using a condom correctly in all circumstances.
Advantages of Health Belief Model (HBM):
- Acknowledges and addresses cognitive model, which lays emphasis on the role of motivations and faith on the individual.
- Publicizes a person’s opinions into four kinds: perceived susceptibility, perceived susceptibility, perceived severity, perceived benefits, and perceived barriers.
- This comprehensive methodology scrutinizes a person’s beliefs, opinions, and views particularly in respect to health care in a further holistic approach in contrast with other models.
- It familiarizes theories from behavior disciplines to inspect health complications.
- It clarifies and expects health conducts.
Limitations of Health Belief Model (HBM):
- As a psychological model it does not take into consideration other factors, such as environmental or economic factors, that may influence health behaviors.
- It does not explain the behaviors that are routine and consequently may possibly inform the decision-making process to accept an acclaimed action (e.g., smoking).
- The model lacks explanations for a person’s attitudes, beliefs, or another individual contributing factor that dictate a person’s approval or acceptance of health behavior.
- HBM does not proceed into the interpretation of behaviors that are executed for non-health connected motives such as social acceptability.
- It does not account for environment friendly or cost-effective factors that may forbid or encourage the suggested action.
- The model does not incorporate the influence of social norms and peer influences on people’s decisions regarding their health behaviors.
- Adopts that cues to action are extensively predominant in positive people to act and that “health” actions are the key objective in the decision-making course.
- Lack of clarification on accessibility and economic access to health care. Example: Many people with serious health illness lack health insurance due to the pre-existent situations.
References and For More Information:
https://www.verywellmind.com/health-belief-model-3132721
https://www.verywellmind.com/health-belief-model-3132721
https://www.enotes.com/homework-help/what-strengths-weaknesses-health-belief-model-252015