Table of Contents
What is Jaundice?
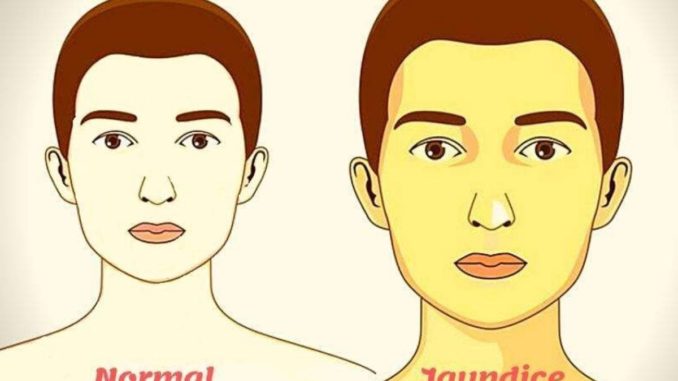
- Jaundice is a condition in which the skin, whites of the eyes and mucous membranes turn yellow because of a high level of bilirubin.
- Jaundice is a yellow coloring of the skin, mucus membranes and eyes.
- Jaundice, also known as ‘icterus’ is a clinical sign of high serum bilirubin.
- The accumulation of high serum bilirubin results in this condition where the skin, mucous membranes, and sclera (the whites of the eyes) to turn yellow.
- The yellow coloring comes from the bilirubin, a byproduct of old red blood cells.
- The liver secretes a fluid called bile and red blood cells are broken down to produce bilirubin.
- Jaundice becomes clinically evident when blood bilirubin levels rise to or above 3 mg/dL.
Key Facts
- According to epidemiology statistics, jaundice incidence varies depending on the underlying cause and is more prevalent in particular age groups.
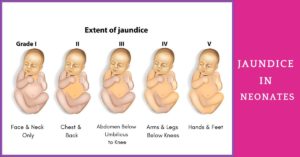
- Jaundice, specifically, affects roughly 6 out of 10 otherwise healthy neonates, mostly because hepatic conjugation and absorption are immature.
- Men are more likely to experience both alcoholic and nonalcoholic liver disease-related jaundice, while women are more likely to experience primary biliary cholangitis as the underlying cause.
- The incidence of jaundice varies depending on the patient group; it is more prevalent in neonates and the elderly.
- Kernicterus, also known as bilirubin-induced neurologic dysfunction (BIND), is an extremely uncommon cause of neonatal death with a mortality incidence of 0.28 per one million live births. It is a consequence of severe jaundice.
Types of Jaundice
There are mainly three types of jaundice:
- Prehepatic: It occurs before the liver processes the waste and leads to higher conjugated bilirubin levels.
- Hepatic: It occurs in the liver and leads to both higher conjugated and unconjugated bilirubin levels.
- Post-hepatic: It occurs after the liver has processed the waste and results in higher conjugated bilirubin levels.

Causes of Jaundice
Jaundice may result due to problem in any one of the three steps of bilirubin production.
- Prior to bilirubin production, jaundice (also known as unconjugated jaundice) may be caused by:
- The reabsorption of a large hematoma (a collection of clotted or partially clotted blood under the skin)
- Hemolytic anemia (blood cells are destroyed and removed from the bloodstream before their normal lifespan is over)
- When bilirubin is produced, jaundice could result from:
- Hepatitis A, chronic Hepatitis B and C, and Epstein-Barr virus infection are examples of viruses (infectious mononucleosis).
- Autoimmune illnesses.
- Rare metabolic genetic abnormalities.
- Prescription drugs, such as acetaminophen toxicity, penicillins, oral contraceptives, chlorpromazine, and anabolic or estrogenic steroids.
- Following the production of bilirubin, obstruction (blockage) of the bile ducts may cause jaundice from:
- Gallbladder inflammation (swelling)
- Bile duct cancer
- Tumor in the pancreas
Other possible causes and conditions include:
- Gallstone disease
- Hepatitis or liver cirrhosis
- Cirrhosis
- Excessive alcohol consumption
- Pancreatic cancer
- Hemolytic anemia
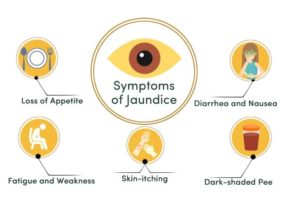
Symptoms of Jaundice
- Pale stools
- Mucous membranes, and the whites of the eyes with a yellow tint
- Dark urine
- Itchiness
- Chills
- The yellowish tint can begin at the head in neonates and progress all the way down the body to the toes.
Other-related symptoms may also include:
- Weariness
- Nausea
- Vomiting
- Fever
- Abdominal pain
Risk Factors
Premature birth:
- It’s possible that a baby born before 38 weeks of pregnancy won’t be able to metabolize bilirubin as quickly as a baby born at term.
- Moreover, premature infants may consume less and have fewer bowel movements, which results in less bilirubin being excreted in the stool.
Significant bruising after delivery:
- Because more red blood cells are broken down during delivery, babies with bruises may have higher levels of bilirubin.
Blood group:
- If the mother’s blood type differs from that of her baby, the newborn may have acquired antibodies through the placenta, which would cause an abnormally rapid breakdown of red blood cells.
Breast-feeding:
- Babies who are breastfed are more likely to develop jaundice, especially if they have trouble nursing or aren’t getting enough nutrients.
- The development of jaundice increase the risk of dehydration or a low calorie intake. Despite this, experts continue to support breastfeeding due to its benefits.
- Ensuring sure baby consumes enough food and water is essential.
Race:
- Studies show that newborns of East Asian descent are more likely to develop jaundice.
Diagnosis
- Bilirubin tests: Higher levels of unconjugated bilirubin compared to conjugated bilirubin are indicative of hemolytic jaundice.
- The complete blood count (CBC) or full blood count (FBC): This gauges the quantities of platelets, white blood cells, and red blood cells.
- Tests for hepatitis A, B, and C: They check for various liver infections.
Complications/Side Effects of Jaundice
- Some of the common side effects are:
- Constipation
- Bloating
- Vomiting
- Diarrhea
- Stomach pain
- Furthermore, the bilirubin can cause potentially fatal damage to the brain and spinal cord.
- Bilirubin encephalopathy is the term used to describe brain damage brought on by excessive bilirubin levels.
- Before receiving treatment, a child who has major brain damage may experience serious and persistent problems like:
- Cerebral palsy
- Loss of hearing
- Having trouble learning
- Problems with their body twitching involuntarily in various places keeping regular eye movements
- Tooth development problems
Prevention
- Jaundice is associated with poor liver function.
- There are several strategies to change one’s way of life to boost liver health, including:
- Maintaining a healthy diet
- Regular exercise
- Avoiding pollutants from chemicals and other sources, both when inhaled and touched,
- Controlling medication carefully
- Limiting alcohol consumption
Treatment of Jaundice
- Jaundice in adults is typically left untreated but the doctor will treat the underlying cause.
- Jaundice will naturally disappear as the liver starts to recover. If the problem is a blocked bile duct, a doctor might advise surgery to clear it.
References and For More Information
https://www.ncbi.nlm.nih.gov/books/NBK544252/
https://www.aafp.org/dam/brand/aafp/pubs/afp/issues/2004/0115/p299.pdf
https://www.webmd.com/hepatitis/jaundice-why-happens-adults
https://www.mayoclinic.org/diseases-conditions/infant-jaundice/symptoms-causes/syc-20373865
https://www.nhs.uk/conditions/jaundice/
https://www.karger.com/Article/Pdf/517301
https://www.cdc.gov/ncbddd/jaundice/facts.html
https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-6-19