Table of Contents
What is Postpartum Depression?
- Postpartum depression is a depression that occurs in female during the postpartum period.
- Postpartum depression refers to the type of depression that takes place in mothers after the child birth.
- Postpartum depression (PPD) is also known as postnatal depression
- Postpartum is the term used to describe the time after childbirth.
- Some women have postpartum depression (PPD), which is a complicated combination of behavioral, emotional, and physical changes.
- The DSM-5, a manual used to identify mental disorders, classifies PPD as a type of serious depression that starts in women within 4 weeks of giving birth.
- PPD is diagnosed based on the severity of the condition and the interval between delivery and beginning.
Facts About Postpartum Depression
- Up to 1 in 5 women will suffer from maternal mental health disorder like postpartum depression.
- Less than 15% of women will receive treatment during this period.
- One in seven women will experience depression during pregnancy.
- Up to 50% of women living in poverty will suffer from a maternal mental health disorder.
- Maternal mental health disorders impact the whole family, not just women .
- In the United States (U.S.), more than 600,000 women will suffer from a maternal mental health disorder every year.
- Anxiety and depression have increased by 37% in teen girls. This number will increase the number of women suffering from PPD in the future.
- Rates of depression are more than doubled in black moms.

Types of Postpartum depression
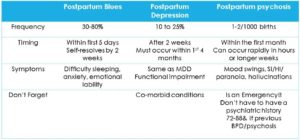
1. Baby blues
- After giving birth, between 50% and 75% of people experience the baby blues.
- You can have abrupt mood fluctuations, such as feeling extremely pleased then extremely sad.
- You might cry without reason and experience irritability, crankiness, restlessness, anxiety, loneliness, and sadness.
- After delivery, the baby blues could persist anywhere from a few hours to 1 to 2 weeks.
- Despite the unpleasantness of the situation, it normally goes away on its own after two weeks.
2. Postpartum depression
- About 1 in 7 new parents experience postpartum depression, a much more dangerous disorder than the baby blues.
- If you’ve previously experienced PPD, your risk rises to 30% with each pregnancy.
- Similar feelings to the baby blues, including as sadness, despair, anxiety, and crankiness, are possible, but you experience them much more intensely.
- Mild to severe symptoms may start to show up a week after delivery or gradually, even up to a year later.
- Despite the seriousness of PPD, it is treatable with medication and counseling.
3. Postpartum psychosis
- A very severe form of postpartum depression that necessitates immediate medical intervention is postpartum psychosis.
- Only 1 in 1,000 people after delivery are affected by this illness, making it very uncommon.
- Severe agitations, confusion, feelings of hopelessness and shame, insomnia, paranoia, hallucinations or delusions, hyperactivity, quick speech, or mania are some of the symptoms.
- Due to the heightened risk of suicide and potential injury to the child, postpartum psychosis requires rapid medical intervention.
- Medication, counseling, and hospitalization are frequently used as treatments.
Causes and Risk Factors
The cause of postpartum depression is not fully clear.
Following are some of the factors that may increase the risk of postpartum depression:
- History of depression before being pregnant or while carrying a child
- Age when the pregnancy began (the younger you are, the higher the chances)
- Uncertainty regarding the pregnancy
- Children (the more you have, the more likely you are to be depressed in a later pregnancy)
- An inheritance of mood problems
- Lack of close family and friends to support
- Experiencing a highly stressful occurrence, such as a job loss or health problem
- Stressful events in family and society
- Having a child with medical issues or unique needs
- Having triplets or twins
- Depression or premenstrual dysphoric disorder in the past (PMDD)
- Insufficient social support
- Being single parent
- Marital conflict
PPD doesn’t have a single cause, but a number of psychological and emotional disorders may contribute to it:
Hormones
- The sharp decline in progesterone and estrogen following childbirth may be a factor.
- Your thyroid gland’s other hormone production may also experience a significant decline, leaving you feeling worn out, lethargic, and depressed.
Sleep deprivation
- When you’re exhausted and sleep deprived, you could find it difficult to deal with even simple issues.
Anxiety
- You might be worried about being able to take care of a newborn.
Self-image
- You can feel less attractive, have identity issues, or lack a sense of control over your life. Any one of these problems may be a factor in postpartum depression.

Symptoms
- Sadness, worthlessness, hopelessness, or guilt
- Overly worrying or being tense
- Loss of interest in past interests or hobbies
- Appetite changes or not eating
- Loss of motivation and energy
- Lack of energy and feeling tired all the time
- Having trouble falling asleep or constantly wanting to sleep
- Crying excessively or without cause
- Lack of interest to socialize and meet people
- Feelings of anger
- Thinking or concentration challenges
- Suicidal ideas or wishes to die
- Lack of interest in your child or unease around your child
- Thoughts of harming your child or feelings of dissatisfaction with having a child
Postpartum Depression in Fathers
- New fathers can experience postpartum depression, too.
- They may feel sad or tired, overwhelmed, anxious, or have changes in their typical eating and sleeping routines, which are symptoms similar to women suffering from PPD.
Consequences and Effect of Postpartum Depression on Baby
- Delayed development of the brain and language
- Poorer grades in school
- An unorganized or insecure attachment and more behavioral issues
- Greater incidence of depression among children in the latter teen years
- Problems with eating and sleeping.
- Obesity and developmental problems are more likely to occur
- Inadequate social skills
Consequences and Effect of Postpartum Depression on Mothers
- Loss of work productivity
- Isolation from friends and family
- Inability to perform daily tasks
- Weight gain or loss
- Self-harm
- Suicide
- Impaired mother-infant bond
Preventing Postpartum Depression
PPD can be somewhat avoided. Knowing the condition’s warning signals and the factors that raise your risk is useful.
Here are some suggestions for preventing postpartum depression:
- Ask for help
- Inform people of how they can assist you.
- Be reasonable in your expectations for the baby and for yourself.
- Exercise while adhering to whatever limitations your doctor may impose on your level of activity; go for a walk to get some fresh air.
- Be prepared for both happy and terrible days.
- Adopt a healthy diet and stay away from coffee and alcohol.
- Make time for your partner to strengthen your bond.
- Don’t cut yourself apart from family and friends; stay in touch with them.
- When you first return home, limit visitors.
- Examine incoming calls.
- When your infant sleeps, you should also rest.
Solution and Treatment
- In some cases, PPD goes away on its own within three months after giving baby.
- However, you should seek therapy if it ever interferes with your daily life or if “the blues” persist for more than two weeks.
- Medication, or a combination of medication and psychotherapy, can successfully treat about 90% of women with PPD.
- Hospitalization might be required in cases of severe postpartum depression or postpartum psychosis.
- Electroconvulsive (ECT) therapy may occasionally be used to treat severe depressions with hallucinations, delusions, or overpowering suicidal thoughts if symptoms are particularly severe.
- The initial stage in treatment is to deal with immediate issues such changes in appetite and sleep.
- If the mother is breastfeeding, the doctor and patient must carefully consider the use and selection of antidepressants.
References and For More Information
https://www.webmd.com/depression/guide/postpartum-depression
https://www.mayoclinic.org/diseases-conditions/postpartum-depression/symptoms-causes/syc-20376617
https://www.cdc.gov/reproductivehealth/features/maternal-depression/index.html
https://www.nhs.uk/mental-health/conditions/post-natal-depression/overview/
https://www.womenshealth.gov/mental-health/mental-health-conditions/postpartum-depression#:~:text=%E2%80%9CPostpartum%E2%80%9D%20means%20the%20time%20after,you%20may%20have%20postpartum%20depression
https://my.clevelandclinic.org/health/diseases/9312-postpartum-depression
https://www.postpartumdepression.org/postpartum-depression/types/https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6492376/