
Table of Contents
What is Rabies?
- Rabies is a vaccine-preventable, zoonotic, viral disease.
- Rabies is the deadliest virus that spread to people and pets if they are bitten or scratched by a rabid animal.
- Rabies is a fatal but preventable viral disease.
- Rabies spreads in people from the saliva of the infected animals.
- Rabies is a dangerous virus that affects the central nervous systems and causes brain inflammation in humans and other mammals
- Once clinical symptoms appear, fatality rate of rabies is 100%
- In 99% of the cases, rabies is transmitted to the humans through domestic dogs.
- Rabies is one of the oldest known viral disease-causing encephalitis with cases dating back from 4000 years ago
- For the vast majority of human existence, a bite from rabid animals was fatal and the fear was so much that people would commit suicide if they were bitten by rabid animals
- The development of vaccine by Louis Pasteur in 1885 dramatically changed the natural history of rabid contact at least in the developed countries
- Despite the monumental development taking long back with current development of 3 vaccines, about 30,000 to 70,000 people die annually from rabies.
Key Facts About Rabies

- Rabies is a vaccine-preventable viral disease which occurs due to transmission by an animal bite carrying the infection and is prevalent in more than 150 countries and territories.
- About 99% of all rabies transmission to human are from dogs. Therefore, dogs are the major source of rabies death.
- In countries like United States, rabies is mostly found in wild animals like bats, racoons, skunks,
- As it is a vaccine preventable disease, interrupting transmission is feasible through vaccination of dogs and prevention of dog bites.
- Every year, more than 29 million people worldwide receive a post-bite vaccination.
- Symptoms includes neurological problems and a fear of light and water.
- About 10000 deaths occur every year, mainly in Asia and Africa.
- 40% of people bitten by suspect rabid animals are children under 15 years of age.
- Anyone who receives a bite should seek immediate treatment. Crucial step of immediate, thorough wound washing with soap and water after contact with a suspect rabid animal can save lives
- Multiple sector engagement and collaboration through community education, awareness programmes and vaccination campaigns are critical.
- WHO has led the collective “United against Rabies” to drive progress towards “Zero human deaths from dog-mediated rabies by 2030”.
Some Misconceptions About Rabies
- Rabies isn’t preventable and curable
- It is only transmitted by animal bites
- Indoor dogs and cat don’t need rabies vaccination
- Animals will appear rabid and unwell
- Rabies vaccine can be taken only after bitten by rabid dogs
Causative Agent of Rabies
- Rabies is caused by bullet-shaped RNA rhabdovirus of genus Lyssavirus
Mode of Transmission
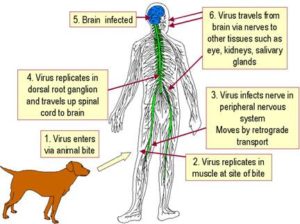
- Rabies is transmitted by bite or scratch from rabid animals
- Transmission can also occur if there is any direct contact of the saliva of infected animals with human mucosa or fresh skin wounds
- Solid organs or tissue allotransplantation have also been documented to transfer rabies
Incubation Period
The incubation period for rabies is typically 2–3 months.
However, it may vary from 1 week to 1 year, depending upon factors such as the location of virus entry and viral load.
Signs and Symptoms of Rabies
- Earliest symptoms of rabies include a fever with pain and unusual or unexplained tingling, pricking, or burning sensation (paraesthesia) at the wound site
- Symptoms eventually progress to cerebral dysfunction, anxiety, confusion and agitation
- As the disease develops, the person may experience delirium, abnormal behavior, hallucinations, hydrophobia and insomnia
- Human survival from clinical service has been documented to be less than 20 cases.
- Furthermore, symptoms of rabies differ according to its forms.
- Usually there are two forms of rabies with different symptoms:
1. Furious rabies:
- It results in hyperactivity, excitable behavior, hydrophobia (fear of water), aerophobia (fear of fresh air).
- In this case, death occurs after few days due to cardio-respiratory arrest.
2. Paralytic rabies:
- It accounts for 20% of total human cases.
- It runs for a longer period than the furious rabies.
- Here, muscles gradually become paralyzed, coma slowly develops and eventually death occurs.
Prevention of Rabies
- Vaccinating dogs are the most cost-effective strategy for prevention of rabies in human as well as animals
- Education on dog behavior and bite prevention for both children and adults can reduce the incidence of rabies
- Pre-exposure immunization of the people who are in the high risk zone. Also the immunization of children should be considered
- Keeping the pets confined and protecting them from predators
- Reporting the stray animals to local authorities and proper management by them should be done
- Access to medical care should be enhanced for the people who gets bitten
- Strong surveillance and monitoring system to check the prevalence of the rabies and to take immediate action if cases seen
Treatment of Rabies
- There is no treatment for rabies but symptomatic and palliative supportive care can be given such as wound care
- Post-exposure prophylaxis (PEP) should be provided immediately after the bite from rabid animals
- This include immediate washing of the wounds and a course of potent and effective rabies vaccine that meets WHO standards
WHO Response to Rabies
- WHO leads the collective “United Against Rabies” to drive progress towards “Zero human deaths from dog-mediated rabies by 2030”.
- WHO’s new road map 2021-2030 include rabies too which requires close cross-sectorial coordination at the national, regional and global levels for its management
- A multi-stakeholder platforms ‘United against Rabies Forum’ (UAR), have been launched that advocates and prioritizes investments in rabies control. Progress in rabies elimination provides an indicator of One Health operationalization and strengthened human and animal health systems
- One Health can truly provide a framework in which cross-cutting benefits can be realized and shared.
- WHO works with partners so that it be a guidance and support countries as they develop and implement their national rabies elimination plans
- WHO regularly updates and disseminates technical guidance on rabies , for example on epidemiology, surveillance, diagnostics, vaccines, safe and cost-effective immunization
- While moving on the path towards rabies elimination countries can request WHO validation of achieving zero human deaths from dog-mediated rabies
References and For More Information
https://www.who.int/news-room/fact-sheets/detail/rabies
https://www.cdc.gov/rabies/index.html
https://www.mayoclinicproceedings.org/article/S0025-6196(11)62291-X/fulltext
https://www.oie.int/en/disease/rabies/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6126826/
https://www.academyanimal.com/news/myths-vs-facts-about-rabies
https://www.iamat.org/blog/5-misconceptions-about-rabies/
https://www.cdc.gov/rabies/medical_care/index.html
https://www.mayoclinic.org/diseases-conditions/rabies/symptoms-causes/syc-20351821
https://www.medicalnewstoday.com/articles/rabies